
Public Health England (PHE) compares the UK’s performance to the UNAIDS 90-90-90 target, whose aim is that countries should have 72.9% of their people with HIV diagnosed, in care and virally suppressed by 2020. The UK has in fact already reached the subsequent UNAIDS 95-95-95 target of 85.7% of people virally suppressed – an estimated 87% of people with HIV in the country have an undetectable viral load. While ‘only’ 92% of people with HIV are diagnosed, 98% of those diagnosed are in care and 97% of those in care are virally suppressed.
During 2017, new diagnoses among all people fell by 17% on the previous year. In gay men they have fallen from 3390 in the peak year of 2015 to 2330 in 2017 – a 32% decline, as already reported on aidsmap.com. Diagnoses have fallen relative to 2016 in every area of the UK, with a particularly sharp fall in Wales. The exception is Northern Ireland, but numbers there are low and this region has also experienced a significant decline in diagnoses since 2011.
Diagnoses have fallen among every sexuality, gender and ethnicity group, not just in white gay men. There are two groups among whom a fall in diagnoses is new. One is white heterosexuals – diagnoses among men fell 31% and among women by 16%, relative to 2016. The other is black and minority-ethnic gay men, in whom diagnoses were previously not falling. Last year, they fell by 57% in black men, 22% in Asian men (where they had been significantly increasing), and 36% among other/mixed ethnicities. Diagnoses also fell among heterosexuals of African and Caribbean ethnicity who were born in the UK.
The numbers of people diagnosed late, with a CD4 count of below 350 cells/mm3, also fell. The decline was most marked among black African women and men (decreases of 82% and 79% since 2008, respectively). However, as reported previously, these absolute declines are largely because of a fall in all diagnoses and 52% of African heterosexual women and 69% of men are diagnosed late, compared with 52% of white heterosexuals and 33% of gay men. A quarter of those diagnosed late are diagnosed with CD4 counts below the AIDS-defining limit of 200 cells/mm3.
Probably more impressive even than the decline in diagnoses is the decline in the actual number of new infections – incidence. This is estimated with data from the 47% of new diagnosed people who have a recency (RITA) test, which can detect infections acquired in the last six months, as well as CD4 back-calculation, which computes date of infection from average CD4 count decline.
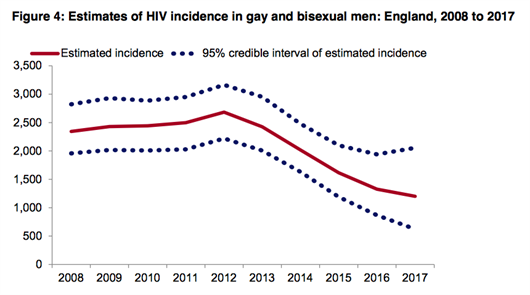
PHE estimates that last year there were most likely about 1200 new infections in gay and bisexual men (with a range of uncertainty between 600 and 2100), which is a reduction of 56% from the estimated peak of 2700 in 2012. Only 286 men tested with RITA showed evidence of infection in the last six months.
The proportion testing positive who had recent infection rose to a peak of 36% in 2014 but has since declined. This is revealed indirectly by the ratio of new infections to new diagnoses. In 2012-2015 the majority of diagnoses in gay men were of recent infections, with a ratio of 0.8 new infections per diagnosis, but it is now down to 0.5.
In other words, increased testing initially uncovered a lot of recent infections but with the further increase in testing and viral suppression, the proportion of infections diagnosed that are recent has now fallen. More infections diagnosed are now of chronic infections that people have been living with for several years.
PHE do not provide incidence estimates for other groups as fewer are tested with RITA and the uncertainty is greater.
